Antimicrobial resistance
Antimicrobial resistance (AMR) occurs when microorganisms no longer respond to treatment with antimicrobial medicines. This is a natural phenomenon that occurs over time through genetic changes in microorganisms. However, the rate at which this occurs is strongly accelerated by the inappropriate use of antimicrobial medicines.
There are different types of antimicrobials, which work against different types of microorganisms, such as antibacterials or antibiotics against bacteria, antivirals against viruses, and antifungals against fungi.
Because of growing resistance, the world is running out of effective antimicrobials to treat infections. Standard treatments become ineffective, infections become harder or impossible to treat, and other medical procedures and treatments – such as surgery or cancer chemotherapy – become much riskier.
Unless appropriate action is taken, decades of progress in health and medicine will be jeopardized.
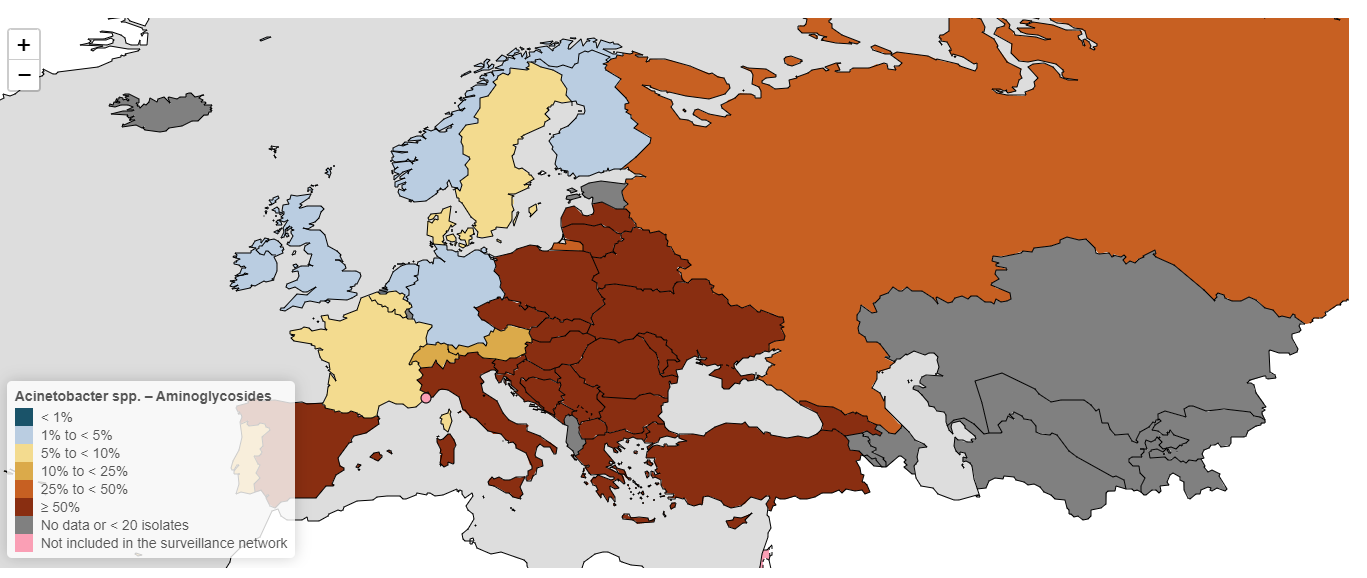
Antimicrobial resistance (AMR) is one of the top global health threats of our time, potentially reversing significant medical breakthroughs of the past century. AMR is leading to substantial increases in deaths and disease burden in the WHO European Region.
Globally, every year, over 1 million people die directly from AMR and nearly 5 million deaths are indirectly linked to AMR.
In the WHO European Region, AMR is directly responsible for 133 000 deaths each year and indirectly linked to 541 000 deaths. This corresponds to the disease burden of tuberculosis, influenza and HIV/AIDS combined.
Estimates show that AMR costs the European Union and European Economic Area about €11.7 billion each year due to increased health expenditure and workforce productivity losses.
AMR is accelerated by the inappropriate use of antimicrobial medicines.
WHO/Europe is supporting countries to address the threat of antimicrobial resistance (AMR) by:
- providing technical guidance;
- performing national assessments and supporting national action plan development;
- supporting health leadership and regional policy development;
- facilitating intersectoral collaboration;
- providing training and building capacity;
- publishing the latest surveillance data;
- monitoring the implementation of the “Roadmap on antimicrobial resistance for the WHO European Region 2023–2030”;
- supporting advocacy and public-awareness raising.
WHO/Europe works with countries across all topics relevant to AMR, such as:
- surveillance of antimicrobial resistance and consumption
- antimicrobial stewardship
- infection, prevention and control
- water, sanitation and hygiene
- awareness and behaviour change
- laboratory quality management
- food safety.